Article type: Literature Review
Article title: Deep brain stimulation for the management of refractory neurological disorders: A comprehensive review
Journal: Medicina
Year: 2023
Authors: Jamir Pitton Rissardo, Nilofar Murtaza Vora, Irra Tariq, Amna Mujtaba and Ana Letícia Fornari Caprara
E-mail: jamirrissardo@gmail.com
ABSTRACT
In recent decades, deep brain stimulation (DBS) has been extensively studied due to its reversibility and significantly fewer side effects. DBS is mainly a symptomatic therapy, but the stimulation of subcortical areas by DBS is believed to affect the cytoarchitecture of the brain, leading to adaptability and neurogenesis. The neurological disorders most commonly studied with DBS were Parkinson’s disease, essential tremor, obsessive-compulsive disorder, and major depressive disorder. The most precise approach to evaluating the location of the leads still relies on the stimulus-induced side effects reported by the patients. Moreover, the adequate voltage and DBS current field could correlate with the patient’s symptoms. Implantable pulse generators are the main parts of the DBS, and their main characteristics, such as rechargeable capability, magnetic resonance imaging (MRI) safety, and device size, should always be discussed with patients. The safety of MRI will depend on several parameters: the part of the body where the device is implanted, the part of the body scanned, and the MRI-tesla magnetic field. It is worth mentioning that drug-resistant individuals may have different pathophysiological explanations for their resistance to medications, which could affect the efficacy of DBS therapy. Therefore, this could explain the significant difference in the outcomes of studies with DBS in individuals with drug-resistant neurological conditions.
Keywords: DBS; movement disorder; brain stimulation; electrical stimulation; IPG; Parkinson’s disease; tremor; symptomatic; neurosurgery; neurology
Full text available at:
DOI
10.3390/medicina59111991
Citation
Rissardo JP, Vora NM, Tariq I, Mujtaba A, Caprara ALF. Deep Brain Stimulation for the Management of Refractory Neurological Disorders: A Comprehensive Review. Medicina 2023;59:1991.
Figure 1. Cortico-basal-ganglia-thalamo-cortical circuitry. The direct, indirect, and hyperdirect pathways are indicated. Green lines denote inhibitory connections (GABAergic), red lines denote excitatory connections (glutamatergic), black lines denote dopaminergic pathways, and blue lines denote mixed cholinergic connections. Notably, the pedunculopontine nucleus (PPN) exhibits anatomic projections to the striatum and cortex. Abbreviations: D1, dopamine receptor D1; D2, dopamine receptor D2; GPe, external globus pallidus; GPi, internal globus pallidus; PPN, pedunculopontine nucleus; SNC, substantia nigra pars compacta; SNr, substantia nigra pars reticulata; STN, subthalamic nucleus.
Figure 2. Modes of stimulation. The monopolar (cathodic) stimulation has a spreading negative current in all directions. In the bipolar, the electrode has both anodic and cathodic contact points, with a narrower and more intense flow of current between them.
Figure 3. The main targets of deep brain stimulation for the management of chronic pain.
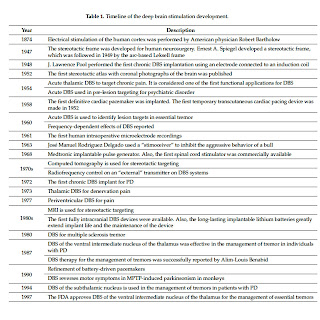
Table 1. Timeline of the deep brain stimulation development.
Table 2. Stimulus-induced side effects in DBS surgical procedures.
Table 3. Features of implantable pulse generators for deep brain stimulation.
Table 4. Clinical trials of deep brain stimulation.
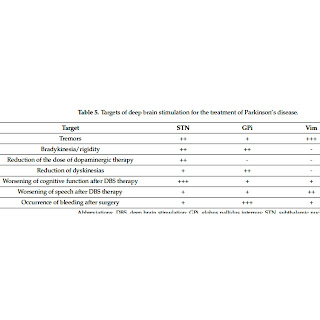
Table 5. Targets of deep brain stimulation for the treatment of Parkinson’s disease.