Article type: Literature Review
Article title: Flapping Tremor: Unraveling Asterixis-A Narrative Review
Journal: Medicina
Year: 2024
Authors: Jamir Pitton Rissardo, Sara Muhammad, Venkatesh Yatakarla, Nilofar Murtaza Vora, Paras Paras, and Ana Letícia Fornari Caprara
E-mail: jamirrissardo@gmail.com
ABSTRACT
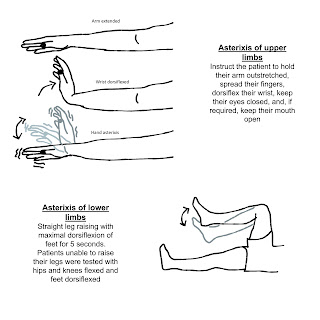
Asterixis is a subtype of negative myoclonus characterized by brief, arrhythmic lapses of sustained posture due to involuntary pauses in muscle contraction. We performed a narrative review to characterize further asterixis regarding nomenclature, historical aspects, etiology, pathophysiology, classification, diagnosis, and treatment. Asterixis has been classically used as a synonym for negative myoclonus across the literature and in previous articles. However, it is important to distinguish asterixis from other subtypes of negative myoclonus, for example, epileptic negative myoclonus, because management could change. Asterixis is not specific to any pathophysiological process, but it is more commonly reported in hepatic encephalopathy, renal and respiratory failure, cerebrovascular diseases, as well as associated with drugs that could potentially lead to hyperammonemia, such as valproic acid, carbamazepine, and phenytoin. Asterixis is usually asymptomatic and not spontaneously reported by patients. This highlights the importance of actively searching for this sign in the physical exam of encephalopathic patients because it could indicate an underlying toxic or metabolic cause. Asterixis is usually reversible upon treatment of the underlying cause.
Keywords: asterixis; anisosterixis; mini-asterixis; myoclonus; hyperkinetic; encephalopathy; drug induced; movement disorder
Full text available at:
https://www.mdpi.com/1648-9144/60/3/362
DOI
https://doi.org/10.3390/medicina60030362
Citation
Rissardo JP, Muhammad S, Yatakarla V, Vora NM, Paras P, Caprara ALF. Flapping Tremor: Unraveling Asterixis—A Narrative Review. Medicina 2024; 60:362.