Article type: Literature Review
Article title: A Systematic Review of Oral Vertical Dyskinesia (“Rabbit” Syndrome)
Journal: Medicina
Year: 2024
Authors: Jamir Pitton Rissardo, Krish Kherajani, Nilofar Murtaza Vora, Venkatesh Yatakarla, Ana Letícia Fornari Caprara, Jeffrey Ratliff, and Stanley N. Caroff
E-mail: jamirrissardo@gmail.com
ABSTRACT
Background and Objectives: Vertical rhythmic dyskinetic movements that are primarily drug-induced and affect solely the jaw, mouth, and lips without involving the tongue have been historically described as “rabbit” syndrome (RS). Evidence on the unique features and implications of this disorder remains limited. This literature review aims to evaluate the clinical–epidemiological profile, pathological mechanisms, and management of this movement disorder. Materials and Methods: Two reviewers identified and assessed relevant reports in six databases without language restriction published between 1972 and 2024. Results: A total of 85 articles containing 146 cases of RS were found. The mean frequency of RS among adults in psychiatric hospitals was 1.2% (range 0–4.4%). The mean age of affected patients was 49.2 (SD: 17.5), and 63.6% were females. Schizophrenia was the most frequent comorbidity found in 47.6%, followed by bipolar disorder (17.8%), major depressive disorder (10.3%), and obsessive–compulsive disorder (3.7%). Five cases were idiopathic. The most common medications associated with RS were haloperidol (17%), risperidone (14%), aripiprazole (7%), trifluoperazine (5%), and sulpiride (5%). The mean duration of pharmacotherapy before RS was 21.4 weeks (SD: 20.6). RS occurred in association with drug-induced parkinsonism (DIP) in 27.4% and with tardive dyskinesia (TD) in 8.2% of cases. Antipsychotic modification and/or anticholinergic drugs resulted in full or partial recovery in nearly all reported cases in which they were prescribed. Conclusions: RS occurs as a distinct drug-induced syndrome associated primarily but not exclusively with antipsychotics. Distinguishing RS from TD is important because the treatment options for the two disorders are quite different. By contrast, RS may be part of a spectrum of symptoms of DIP with similar course, treatment outcomes, and pathophysiology.
Keywords: rabbit syndrome; parkinsonism; dyskinesia; tardive dyskinesia; drug-induced; antipsychotic; antidepressant
Full text available at:
DOI
Citation
Rissardo JP, Kherajani K, Vora NM, Yatakarla V, Fornari Caprara AL, Ratliff J, Caroff SN. A Systematic Review of Oral Vertical Dyskinesia (“Rabbit” Syndrome). Medicina 2024;60:1347. https://doi.org/10.3390/medicina60081347.
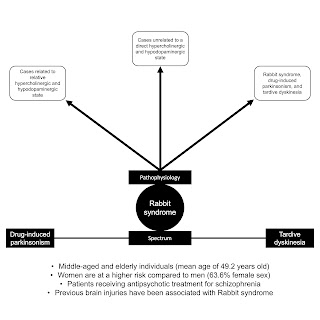
Graphical Abstract. Oral Vertical Dyskinesia (“Rabbit” Syndrome).
Figure 1. Flowchart of the screening process.
Figure 2. Drug-induced parkinsonism, rabbit syndrome, and dyskinesia spectrum. Abbreviations: DIP, drug-induced parkinsonism; DKN, dyskinesia; RS, rabbit syndrome.
Table 1. Frequency of RS among different studies.
Table 2. RS cases associated with medications.
Table 4. Clinical features of RS and TD.