Article type: Literature Review
Article title: Rasmussen Encephalitis: Clinical Features, Pathophysiology, and Management Strategies—A Comprehensive Literature Review
Journal: Medicina
Year: 2024
Authors: Ana Leticia Fornari Caprara, Jamir Pitton Rissardo, Eric P. Nagele
E-mail: jamirrissardo@gmail.com
Year: 2024
Authors: Ana Leticia Fornari Caprara, Jamir Pitton Rissardo, Eric P. Nagele
E-mail: jamirrissardo@gmail.com
ABSTRACT
Rasmussen encephalitis (RE) is a rare and progressive form of chronic encephalitis that typically affects one hemisphere of the brain and primarily occurs in pediatric individuals. The current study aims to narratively review the literature about RE, including historical information, pathophysiology, and management of this condition. RE often occurs in individuals with normal development, and it is estimated that only a few new cases are identified each year in epilepsy centers. Approximately 10% of cases also occur in adolescents and adults. The hallmark feature of RE is drug-resistant focal seizures that can manifest as epilepsia partialis continua. Also, patients with RE usually develop motor and cognitive impairment throughout the years. Neuroimaging studies show progressive damage to the affected hemisphere, while histopathological examination reveals T-cell-dominated encephalitis with activated microglial cells and reactive astrogliosis. The current therapy guidelines suggest cerebral hemispherotomy is the most recommended treatment for seizures in RE, although significant neurological dysfunction can occur. Another option is pharmacological management with antiseizure medications and immunomodulatory agents. No significant progress has been made in understanding the pathophysiology of this condition in the last decades, especially regarding genetics. Notably, RE diagnosis still depends on the criteria established by Bien et al., and the accuracy can be limited and include genetically different individuals, leading to unexpected responses to management.
Keywords: rasmussen encephalitis; rasmussen syndrome; encephalitis; epilepsy; hypometabolism; epilepsia partialis continua; refractory epilepsy; cerebral hemiatrophy
Full text available at:
https://www.mdpi.com/1648-9144/60/11/1858
Citation
Fornari Caprara AL, Rissardo JP, Nagele EP. Rasmussen Encephalitis: Clinical Features, Pathophysiology, and Management Strategies—A Comprehensive Literature Review. Medicina 2024; 60:1858.
Figure 1. The natural history of Rasmussen’s encephalitis.
Figure 2. Schematic diagram of the proposed mechanisms for the drugs related to Rasmussen’s encephalitis management. 1—Inhibition of lymphocyte T proliferation (tacrolimus, mycophenolate mofetil, and azathioprine). 2—Diapedesis blockage (natalizumab). 3—Pro-inflammatory cytokines blockage (adalimumab, anakinra, and infliximab). 4—Antibody blockage/ clearance (intravenous immunoglobulin, plasmapheresis, and adsorption). 5—Inhibition of lymphocyte B proliferation (rituximab). 6—Inhibition of T and B lymphocytes (alemtuzumab, mitoxantrone, cyclophosphamide). 7—Unknown etiology (ganciclovir). 8—Broad-spectrum anti-inflammatory action (corticosteroids).
Figure 3. Management of Rasmussen’s encephalitis. First, surgery eligibility should be assessed. Second, medical treatment can be used independent of the indication of the surgical procedure. The first-line therapies are corticosteroids ± intravenous immunoglobulin (IVIg) ± plasmapheresis/immunoadsorption. Second-line therapies are related to targeting lymphocytes, pro-inflammatory cytokines, and other mechanisms. The data is scarce in providing specific definitions for most second-line therapies in RE.
Table 1. Histological classification proposed by Robitaille et al. (1991)
Table 2. Neuroimaging stages of Rasmussen’s encephalitis proposed by Bien et al. (2005)
Table 4. Critical analysis of cases described by Olson et al. (2013)
Table 5. Medical treatment of Rasmussen’s encephalitis.
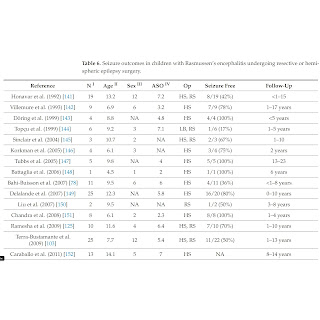
Table 6. Seizure outcomes in children with Rasmussen’s encephalitis undergoing resective or hemispheric epilepsy surgery.
Table 7. Cognitive outcome after hemispherectomy in patients with RE.
Table 8. Differential diagnosis of RE and explorations, adapted from Bien et al. (2005)
Table 9. Neuroimaging of some cerebral hemi-atrophy causes.