Article type: Systematic Review
Article title: Pre- and post-cranioplasty hydrocephalus in patients following decompressive craniectomy for ischemic stroke: a systematic review and meta-analysis
Journal: Neurosurgical Review
Year: 2025
Authors: Ibrahim Khalil, Reem Sayad, Sara K. Kamal, Zainab Hussein, Salma Allam, Ana Letícia Fornari Caprara, Jamir Pitton Rissardo
E-mail: jamirrissardo@gmail.com
ABSTRACT
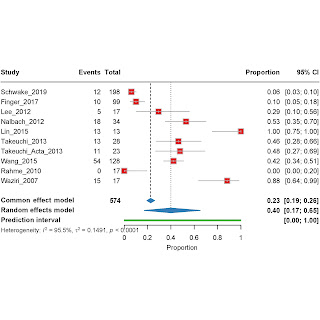
Decompressive hemicraniectomy (DC) for malignant ischemic stroke can lead to hydrocephalus (HC). The dynamics of hydrocephalus at the time of subsequent cranioplasty (CP) are not well characterized. We aimed to systematically review and meta-analyze the rates of hydrocephalus and ventriculomegaly before and after CP, shunt dependency, and hydrocephalus resolution in patients who underwent DC for ischemic stroke. Following the PRISMA guidelines, we searched PubMed, Embase, Scopus, Web of Science, and Cochrane Library through January 2025 (registration number CRD420251039185). in studies reporting hydrocephalus in patients undergoing DC followed by CP for ischemic stroke. Inclusion criteria were ≥ 10 patients in the English language. Data on hydrocephalus/ventriculomegaly rates (pre-CP and post-CP), shunt dependency, and resolution were extracted. Study quality was assessed using the MINORS criteria. Random-effects meta-analyses were performed to calculate pooled proportions with 95% confidence intervals (CI). Heterogeneity was assessed using I², and sources were explored using meta-regression and sensitivity analyses. Ten retrospective studies, involving 579 patients, met the inclusion criteria. The study quality was predominantly fair (6/10) or low (3/10). Pooled rates were: pre-CP hydrocephalus 0.40 (95% CI: 0.17–0.65; I²=95.5%), post-CP hydrocephalus 0.46 (0.14–0.79; I²=89.8%), pre-CP ventriculomegaly 0.43 (0.21–0.67; I²=95.5%), and post-CP ventriculomegaly 0.46 (0.14–0.79; I²=89.8%). There was no significant difference between the pre- and post-CP hydrocephalus rates (P = 0.6481). The pooled rate of shunt-dependent hydrocephalus was 0.11 (0.04–0.22; I²=61.4%), and the hydrocephalus resolution rate post-CP was 0.27 (0.07–0.53; I²=68.7%). Significant heterogeneity was observed across most outcomes, and a potential publication bias was detected. The GRADE assessment indicated very low-to low-quality evidence. Radiographic hydrocephalus or ventriculomegaly is common (approximately 40–46%) both before and after cranioplasty in patients treated with DC for ischemic stroke, with no significant change immediately post-CP identified in this analysis. However, clinically significant hydrocephalus requiring shunting occurs less frequently (approximately 11%). The quality of evidence is limited by the retrospective study design and high heterogeneity. High-quality prospective studies with standardized definitions and follow-up are needed to better understand hydrocephalus dynamics and the impact of cranioplasty timing in this population.
Keywords: hydrocephalus; cranioplasty; decompressive hemicraniectomy; ischemic stroke; shunt.
Full text available at:
DOI
Citation
Khalil I, Sayad R, Kamal SK, Hussein Z, Allam S, Caprara ALF, Rissardo JP. Pre- and post-cranioplasty hydrocephalus in patients following decompressive craniectomy for ischemic stroke: a systematic review and meta-analysis. Neurosurg Rev 2025;48:514. https://doi.org/10.1007/s10143-025-03650-7
Figure 1. PRISMA flow diagram illustrating the study selection process, detailing the identification, screening, eligibility assessment, and final inclusion of studies in the meta-analysis.
Figure 2. Forest plot of the meta-analysis of pre-cranioplasty hydrocephalus rates. Individual study proportions with 95% confidence intervals (CI) are shown, along with the pooled proportion estimate calculated using a random-effects model. The prediction interval (PI) is also indicated.
Figure 3. Forest plot of the meta-analysis of post-cranioplasty hydrocephalus rates. Individual study proportions with 95% CI are shown, along with the pooled proportion estimate calculated using a random-effects model. The PI is also indicated.
Figure 4. Forest plot of the meta-analysis of pre-cranioplasty ventriculomegaly rates. Individual study proportions with 95% CI are shown, along with the pooled proportion estimate calculated using a random-effects model. The PI is also indicated.
Figure 5. Forest plot of the meta-analysis of post-cranioplasty ventriculomegaly rates. Individual study proportions with 95% CI are shown, along with the pooled proportion estimate calculated using a random-effects model. The PI is also indicated.
Figure 6. Forest plot of the meta-analysis of shunt-dependent hydrocephalus rates. Individual study proportions with 95% CI are shown, along with the pooled proportion estimate calculated using a random-effects model. The PI is also indicated.
Figure 7. Forest plot of the meta-analysis of hydrocephalus resolution rates after cranioplasty. Individual study proportions with 95% CI are shown, along with the pooled proportion estimate calculated using a random-effects model. The PI is also indicated.
Figure 8. Meta-regression plot comparing pre- and post-cranioplasty hydrocephalus rates. The plot visualizes the relationship between the two time points across included studies, with the regression line indicating the overall trend and associated p-value for the comparison.
Table 1. Baseline characteristics of studies on hydrocephalus following decompressive craniectomy for ischemic stroke.
Table 2. Assessment of the quality of studies through methodological index for Non-Randomized studies (MINORS).
Table 3. GRADE SUMMARY: hydrocephalus following decompressive craniectomy for ischemic stroke.