General Examination in Neuro-Ophthalmology
Johannes Kepler (1571 – 1630)
- described how light enters the eye and forms on the retina
2) Autorefractor & lensometer
- values are used to correct visual field and OCT parameters
- newer machines can keep contact lens
- verify the "glasses" prescription
> Look at the glasses and see the lens: progressive, trifocals, etc
> Look at both sides
> Look at the eye when glassed: big (far-sight) and small (near-sight)
S (Sphere - SPH) amount of nearsightedness or farsightedness in the eye. A negative value (-2.50) indicates nearsightedness, while a positive value (+1.25) indicates farsightedness.
C (Cylinder - CYL) amount of astigmatism in the eye. A cylinder value of zero means there is no astigmatism, while a positive or negative value (+0.75 or -1.25) indicates the amount of astigmatism.
A (Axis) indicates the orientation of the astigmatism. It is measured in degrees, ranging from 0 to 180 degrees.
- Look at where is the light
- Patient should look at a distant point
> Analyze the structure and size of pupils
> Always look down to up
- direct and indirect
> Never in front of the patient
> Look from down to up
- swing reflex
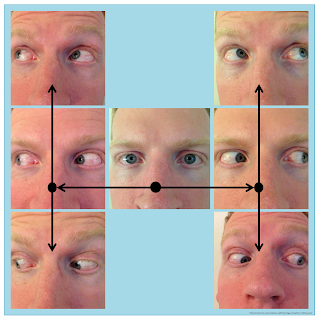
- Horizontal, vertical, diagonal
- Convergence (< 10 cm normal)
- Trace abduction is normal
Obs: saccadic pursuits & nystagmus are a sign of "difficulty"
- Near accommodative triad: “directs his eyes from a distant object to a nearby object” (pupillary accommodation reflex) + (lens accommodation reflex) + (convergence reflex)
- Look at the pencil, close one eye and observe the movement
- do the same with the other eye
- ultimate alternate closing
- Always find the dominant eye, usually right
*If nystagmus, use fog cover (Spielmann occluder). Do not block light because it can increase nystagmus.
> latent nystagmus that occurs when closing eyes
- deviations by nerve problem can be corrected, but muscle can not.
- Ocular acuity with prism ruler for strabismus
- The base of the prism moves eyes to the opposite
> If colorful, reduce the prism
> Look at the movement of the eyes with the prism
9) Visual acuity
- Lorgnette Pinhole Occluder
> First, without pinhole
> If not 20/20 use pinhole
- small aperture allows light to pass through the center of the eye's lens, bypassing defects in its shape
- if you can see better with a pinhole, recommend changing glasses
10) Head position
- Remember to always assess acuity with normal head position, chin up, chin down, and head turn on both sides. Some patients will manifest double vision in specific positions.
- with the chin-down test for both sides to test supranuclear nuclei
- Evaluation of color blindness, one eye at a time
- First and last figures everyone can see the number (functional cases)
- Lang test
> Lang I: 550 – 1200 arc of second
> Lang II: 200 – 600
- number that patient recognize and identify
- other tests: Frisby, Wirt, Randot
- 10 to 21 normal
- change with valsava (do not hold your breath)
AKA: Humphrey visual field
- One eye of a time
> Place autorefractor numbers and correct them according to the indicated len
> Pupil should be at the target
- Normal visual field extends 100° temporally (laterally), 60° nasally, 60° superiorly, and 70° inferiorly
Obs: Always start R, except if the patient has a L-problem. Also, look at the edge of the eye; if there are tears, ask to blink.
Humphrey
- only 30 degrees of visual field
- look at FP & FN
- number is related to size and brightness (big is good)
Hans Goldmann
- explore > 30 degrees of visual field
- performed when Humphrey is unreliable
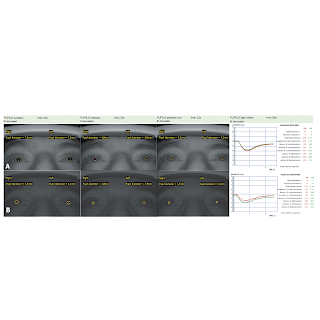
15) Pupillometer
- usually, not billed
- no light followed by a flashlight
- analyze the size and the reaction time in a graph
- analyze RIM width and RNFL of both eyes
> Look at G (global) results
> Look at the graph (if up - edema; if down - atrophy)
- optic neuritis: RIM is ok, problem is RNFL
- PVD can be observed with aging, no important unless detach
- When patient is blind from one eye, you need to use a light object at the side of the other eye for focus
- an aim is placed in the patient’s face
- Up line is horizontal (x), down is vertical (y)
- Test: saccade and pursuit, slow and rapid, and horizontal and vertical, optokinetic nystagmus horizontal and vertical (everyone have, except blind)
- phenylephrine HCl 10%, tropicamide 1% and proparacaine HCl 0.5%
> Phenylephrine - dilates
> Tropicamide - dilates and cycloplegic
> Proparacaine - anesthetic
- Press the lacrimal duct to apply eye drops
19) Slit lamp examination
- anterior segment of the eye
- diopter lens (90D) to see posterior segment of the eye
- fluorescein stain
> Pain & stain means open cornea
- Cataracts
20) Hertel exophthalmometer
- ask about family member eyes
21) External examination
- regarding other neurological findings, including ptosis
> Remember surgery for ptosis
- MG signs
> prolonged upgaze
> Cogan lid
22) Double vision
- If closing one eye does not improve - do not send to neuro-ophthalm, it is a lens problem
- When does it occur? Near and/or far vision
- Always assess MG and thyroid disease
- Letter V (to avoid shadow confusion of other letters)
- Worth 4-dot
> Some patients can alternate suppression ( see 2 red dots and sometimes see 3 green dots)
- Bagolini Glasses
> Patient uses the glasses and a single flashlight is his/her front
(A) orthophoria (or microtropia), (B) suppression of RE, (C) suppression of LE, (D) uncrossed diplopia (esotropia), (E) crossed diplopia (exotropia), and (F) central scotoma without squint.- Double vision when tired or minimal alcohol
> our eyes relax, and convergence is lost
> if convergent insufficiency, do pencil push-up eye exercise to build muscles!
23) Palsies
- most common IV and VI
> Total versus partial (nystagmus, trace)
- can be corrected with prism
- when INO, can be complete versus partial palsy (nsytagmus)
24) Functional blindness
- visual acuity: start with the smallest letter and grow in size (How can't you see?)
- optokinetic evaluation
- prism 35 base down: ask if they can see the top letter
- use a lens (0.5 magnification) (How can't you see?)
- ask for visual field near and far; even in peripheral blind, the field will increase
25) Homonymous hemianopia
- Peli prism lens can correct visual field
26) Pseudopapilledema
- tilted disc
27) Nystagmus
- can be divided: albinism-associated, infantile, and acquired
> congenital is wrong term, infantile because occurs at 2 months of age
- gabapentin, amantadine, 4-aminopyridine (avoid eGFR < 50)
28) Pediatric neuro-ophthalmic eval
- peds are far-sight
- intermittent esotropia is normal (inner eye folds are increased)
- testing eye cover (use the thumb to cover) with animated video
- evaluate movements with a light object (butterfly)
*always do first the lesioned eye, children became upset
- stereo-figures, the child usually touch the figure (only recognition)
- retinoscopy
> use cycloplegic medication
> see streak (red reflex)movement
*move w/ streak - Emmetropia, Hypermetropia, Myopia <1D
*move opposite streak - Myopia >1D
*no movement of streak – Myopia of 1D
> see streak position - refractive error
*astigmatism
- For visual acuity, use Teller acuity cards.
> Look at the eyes moving to the image
> acuity will depend of age, you need the graph
Terms
- Exophoria: one eye drifting uncontrollably outwards. At near is normal.
- Esophoria: eyes to turn inward
- Esotropia: misalignment of eyes, in which one eye deviates towards the nose. A small esotropia around 4 can be corrected by the brain identifying as one object.
- Orthophoria: eyes are perfectly aligned and their lines of vision meet on an object, even when there is no stimulus for fusion
- Oscillopsia: objects in the visual field appear to oscillate. Congenital nystagmus does not cause oscillopsia.
- OU: both eyes
- Synechia: iris adheres to either the cornea